[Event Report] The 120th HGPI Seminar – Necessary Steps for Promoting the Integrated Provision of Palliative Care from Post-diagnosis to End-of-Life With Addressing Cancer Related Pain (October 10, 2023)
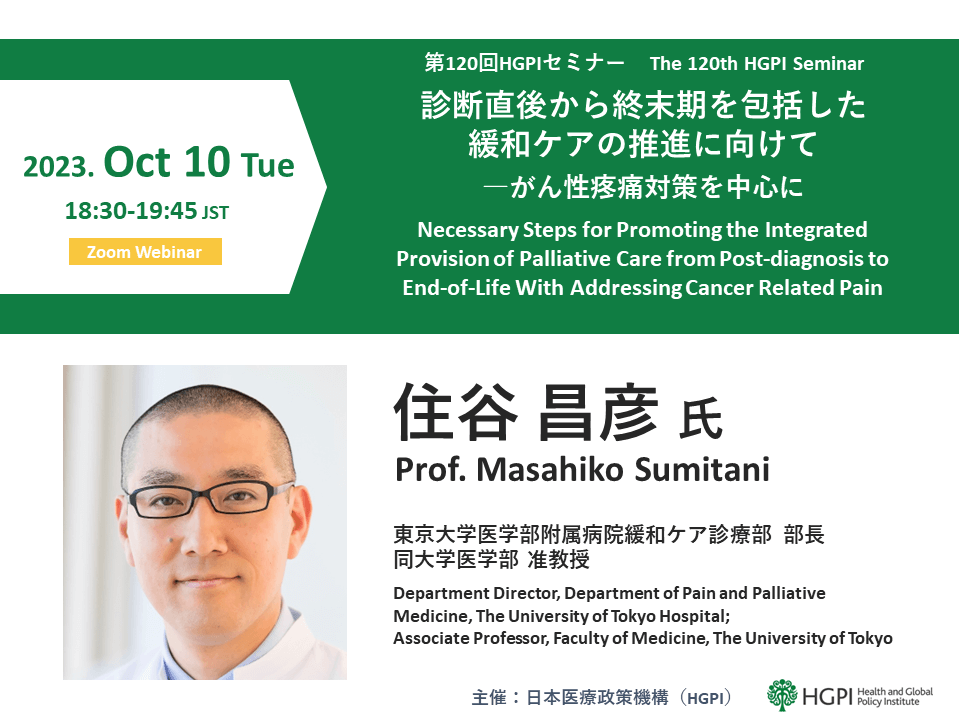 For the 120th HGPI Seminar, we hosted Professor Masahiko Sumitani, Director of the Department of Pain and Palliative Medicine at the University of Tokyo Hospital, who gave a lecture on the growing recognition of the classifications of chronic cancer pain and palliative care and the necessary steps for advancing comprehensive palliative care that encompasses the early post-diagnosis, treatment, and end of life phases as well as care for cancer survivors.
For the 120th HGPI Seminar, we hosted Professor Masahiko Sumitani, Director of the Department of Pain and Palliative Medicine at the University of Tokyo Hospital, who gave a lecture on the growing recognition of the classifications of chronic cancer pain and palliative care and the necessary steps for advancing comprehensive palliative care that encompasses the early post-diagnosis, treatment, and end of life phases as well as care for cancer survivors.
Key points of the lecture
- Palliative care was first introduced to alleviate suffering at the end of life. In recent years, it has expanded to encompass early post-diagnosis and treatment and is contributing to better patient quality of life and improved treatment outcomes.
- Expanding palliative care beyond the end of life phase will require enhancing outpatient palliative care, and expectations for the medical service fee schedule to help this progress occur is high.
- “Opioid crisis” has two meanings. The first refers to the crisis in countries where opioids are overused and many people have died due to its side effects. The second is the crisis in other countries, where misunderstandings toward problems in countries where opioids are overused have resulted in unfounded fear toward opioids and overly-restrictive prescribing practices.
- Disseminating palliative care will require encouraging the appropriate use of opioid analgesics.
- Promoting palliative care and pain control will require educating a wide range of healthcare professionals and providing specialized education on palliative care and pain medicine at universities.
The expansion of the WHO’s classification of cancer-related pain and palliative care
When the World Health Organization (WHO) issued the International Classification of Diseases 11th Revision (ICD-11) in 2018, “cancer pain,” which refers to pain caused by cancer pathology (such as abdominal pain from the invasion of internal organs or metastatic bone pain), was renamed “cancer-related pain,” which encompasses the pain associated with cancer treatment in addition to the pathology of the cancer itself. In addition, the term “palliative care” has historically centered around the terminal phase and has been used to refer to care introduced in the period that spans the functional decline prior to death for patients with advanced cancer. Today, we know that many people with cancer experience pain during treatment, outside of the terminal phase. Many cancer survivors also live with pain. Given this backdrop, the WHO revised its definition of palliative care in 2002 to, “An approach that improves the quality of life (QOL) of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychological and spiritual.”
The need for and effects of palliative care
Standard cancer treatments like radiation therapy, surgery, and drug therapy can result in pain-related complications. For example, drug-induced neuropathy can cause pain and numbness in the feet and hands. It has been reported that such complications lead to reduction, interruption, or discontinuation of drug therapy in up to 17% of cases. Furthermore, patients who experience severe pain have poorer cancer treatment outcomes than those who do not. This is partly because higher grades of cancer may spread more easily and cause more pain. It is also partly because pain associated with cancer treatment can reduce levels of daily activity and volume of food intake, which can prevent people from being able to continue the cancer treatment that is best for them. In the latter scenario, controlling complications can impact treatment outcomes, and it has been shown that providing patients with long-term support from palliative care teams early on leads to better outcomes.
Promoting outpatient palliative care that does not conform to preconceptions centered on the terminal stage
While oncologists at the University of Tokyo Hospital understand why palliative care is necessary, patients and their family members often associate the term “palliative care” with the terminal phase, and this can discourage them from seeking medical examinations. To address this, the University of Tokyo Hospital has established an outpatient service specializing in cancer treatment-related pain at its Pain Clinic, which also provides pain management for forms of pain that are not cancer-related. The term “palliative care” is not used at the Pain Clinic, which helps encourage patients to attend medical examinations.
In the past, palliative care was mainly provided through inpatient services, but promoting outpatient palliative care will be particularly important to advance appropriate palliative care. While some university hospitals have been providing outpatient palliative care in recent years, in many cases, such services are only available on certain days. This has resulted in situations in which cancer specialists were the only healthcare professionals available to follow-up on palliative care for other forms of pain. Furthermore, in the current medical service fee schedule, the only form of outpatient palliative care that is eligible for the premium for outpatient palliative care management is that which is provided by palliative care specialists. However, some people still require palliative care in their communities after being discharged from hospitals and transferred to local healthcare facilities that are more easily accessible. We require a medical service fee reimbursement system that is suitable for such situations.
The uneven distribution of opioids and the two opioid crises
Opioid analgesic use is extremely high in certain countries, such as the United States and Canada, which use 200 to 300 times more opioid analgesics than Japan. This global imbalance was pointed out in a report published by the International Association for the Study of Pain (IASP) in 2022 for the “Global Year for Translating Pain Knowledge to Practice” campaign. Opioid analgesic overuse in certain high-income countries is having adverse effects on countries where access to such pharmaceuticals is still inadequate. These effects include an economic problem in which all of the available pharmaceuticals are bought up by high-income countries, driving up their market value and preventing low- and middle-income countries from being able to purchase them. They also include psychological problems that occur when issues related to opioid side effects in certain high-income countries lead to misunderstandings and unwarranted fear of opioids in other countries.
The term “opioid crisis” refers to circumstances in which many people die due to opioid abuse, and this has become a problem in countries where opioids are overused. Reports of these problems in other countries are causing healthcare professionals and patients to develop misunderstandings that cause them to limit the use of opioids more than is necessary and in an irrational manner. This fear is called “opiophobia” and is recognized as a secondary opioid crisis.
Changes in global discussions surrounding opioids
Situations similar to the secondary opioid crisis have emerged in certain parts of the United States. In 2016, the Centers for Disease Control and Prevention (CDC) issued guidelines to control the use of opioids and prevent overdoses. This led insurers to begin denying coverage for prescriptions that exceed the doses and durations outlined in the CDC’s guidelines, which forced more patients to go without necessary prescriptions. This resulted in a wave of criticism that the guidelines were disadvantageous toward patients, which led the US Department of Health and Human Services (HHS) to issue “Pain Management Best Practices” in 2019 and the CDC to issue new guidelines titled, “2022 Clinical Practice Guideline – Opioids.” These guidelines recommend using opioids appropriately based on the conditions of individual patients after completing a patient-centered decision making process. In a fact sheet issued in 2020, the WHO states that palliative care and the use of opioid analgesics is recognized under the human right to health, and that controlling pain symptoms at early stages is an ethical duty to relieve suffering and to uphold individual dignity.
Domestic palliative medicine consumption and the degree to which palliative care has expanded in Japan
One objective indicator used to assess the adequacy of palliative care is the amount of palliative medicines consumed. The WHO recommends the use of palliative medicines as long as there are no extreme shortages. In Japan, the median amount of palliative medicines used by patients with terminal cancer was 311.0 mg per person. There was a 16-fold regional difference between Yamagata Prefecture, which used the greatest volume, and Tokushima Prefecture, which used the least. While regional variances are problematic, another problem is that Japan only consumes about one-twentieth of the minimum amount of palliative medicines deemed necessary by the WHO. While prescription rates increased slightly from 2010 to 2019, looking at which healthcare facilities provided those prescriptions by number of beds, usage only increased in small hospitals with 199 or fewer beds (where most beds are chronic care and palliative care beds). For hospitals with more beds, the number of prescriptions decreased. As many prefectural core hospitals for coordinated cancer care have 200 beds or more, prescription rates at core hospitals may be decreasing.
Improving this situation will first require getting a grasp on current circumstances. The Ministry of Health, Labour, and Welfare (MHLW) must regularly monitor prescription rates in each prefecture and present their findings. When doing so, it will be important for them to exclude the number of deaths caused by non-medical use of opioids and narcotics, like in the United States. To mount countermeasures against opiophobia in the future, it will also be necessary to survey real-world circumstances surrounding opiophobia among both healthcare professionals and patients.
Making appropriate use of painkillers to meet people’s needs on the individual level
In the past, Japan used a stepwise approach to clinical analgesic usage that followed the WHO’s three-step analgesic ladder, but this approach has gradually shifted toward an elevator method based on the 2018 WHO guidelines on cancer pain management, which call for the direct selection of optimal analgesics according to pain intensity. It is important to keep in mind that opioid analgesic effectiveness is influenced by genetics and can vary from person to person, so one important point of the 2018 Guidelines is that palliative medicines should, in principal, be administered in necessary dosages set on a per-patient basis and without predetermined upper limits.
Recognizing the importance of making appropriate use of palliative medicines tailored to each stage of treatment, the University of Tokyo Hospital created and implemented guidelines titled, “Approach to Chronic Cancer Pain Management.” In this approach, opioids are used proactively to manage pain in cases of advanced cancer. Opioids with high analgesic effects are used in the treatment phase, particularly for cases for which it is considered likely that the patient will suspend treatment due to pain. Otherwise, priority is given to non-opioid analgesics. For pain among cancer survivors, which is very similar to non-cancer-associated chronic pain, pain management is centered around non-opioid analgesics with opioid analgesics prescribed as necessary and on a supplementary basis, in the minimum required doses. These guidelines are consistent with the approach used by the U.S. Department of Health and WHO. They have also been published in a peer-reviewed English-language journal and have been recognized as a reasonable strategy for treatment.
Educating and building awareness among healthcare professionals to disseminate palliative care in the future
According to a study conducted overseas on reasons opioid analgesics do not reach patients who need them, 38% of cases were due to insufficient understanding or training for healthcare professionals. In Japan, training on palliative care for healthcare professionals is provided by the MHLW and the Japanese Society for Palliative Medicine. Most of the people who undergo that training are staff members of core hospitals for coordinated cancer care, but there are signs that suggest opioid prescription rates may be low at core hospitals, so the target audience and structure of palliative care training programs must be reviewed in the future. While the current curriculum includes a variety of content, cancer pain management accounts for approximately 80% of care provided by palliative care teams. One idea may be to place the focus of that curriculum on cancer pain.
Palliative medicine education must also be expanded to include local clinics. Pain is something that changes daily, so great improvements to QOL for cancer patients may be within reach if palliative medicine prescriptions can be adjusted at local clinics that are easier for them to access. Furthermore, when nurses, psychologists, or pharmacists provide medical services and prescribe opioids, the medical service fee schedule requires selecting one for reimbursement, which creates a trade-off among the three. While encouraging suitable interventions among multi-professionals, it will be important to be able to connect patients to physicians who can prescribe opioids appropriately when patients must switch to opioids, so educating multi-professionals will also be important.
Finally, to drive progress in palliative care and pain medicine, it should be mandatory for university hospitals to provide courses on palliative medicine and pain medicine to expand educational opportunities in these fields. In Japan, the number of university hospitals that provide courses in palliative medicine and pain medicine is still limited. Making these courses mandatory is likely to help achieve wide-ranging progress in palliative medicine and pain medicine.
[Event Overview]
- Speaker: Masahiko Sumitani (Department Director, Department of Pain and Palliative Medicine, The University of Tokyo Hospital; Associate Professor, Faculty of Medicine, The University of Tokyo)
- Date & Time: Tuesday, October10, 2023; from 18:30 to 19:45 JST
- Format: Online (Zoom webinar)
- Language: Japanese
- Participation fee: Free
- Capacity: 500
■ Speaker Profile:
Masahiko Sumitani (Department Director, Department of Pain and Palliative Medicine, The University of Tokyo Hospital; Associate Professor, Faculty of Medicine, The University of Tokyo)
Masahiko Sumitani earned MD from the Faculty of Medicine at Tsukuba University. Subsequently, he completed PhD in Medicine at Department of Acute Critical Medicine (Anesthesiology), Osaka University, Graduate School of Medicine. He served as the Assistant professor at Department of Anesthesiology and Pain Relief Center, The University of Tokyo Hospital (2008-2012), the Department Director, Department of Medical Engineering, The University of Tokyo Hospital, and Lecturer, Faculty of Medicine, The University of Tokyo (2012-2014), and has been appointed as Department Director, Department of Pain and Palliative Medicine and Associate Professor at Tokyo University Hospital since 2014.
He also serves for many pain-related academic societies including but not limited to the Japanese Association for the Study of Pain, the Japan Neuroscience Society International Association for the Study of Pain and International Association for the Study of Pain. He has been nominated for a number of awards including Young Investigation Award for Clinical Study of the Japan Society for Clinical Anesthesia (2010).


